Jenna Barton, LPC-T
Also referred to as perinatal mood and anxiety disorders (PMADs), maternal mental health is comprised of a range of mental health disorders that have particular onset during or after pregnancy (up to one year). Women with previous mental health challenges are at higher risk for the development of PMADs but this is NOT a requirement- many women are completely caught off guard by these new challenges. Their symptoms range in varying severity levels of depression, anxiety, and psychosis. Below is a descriptive list of disorders we see across all cultural backgrounds of pregnant women and mothers (and fathers too). PSI (Postpartum Support International) reports that one in 10 dads get postpartum depression and up to 18% develop a clinically significant anxiety disorder). The following is an introduction to postpartum depression and maternal mental health:
• The ‘Baby Blues’- according to the American Pregnancy Association and 2020Mom, the baby blues effects 70-80% of new mothers. Negative feelings, mood swings, sadness, and crying episodes are all symptoms. These symptoms are not considered a disorder as they typically subside after a few days. If these symptoms persist after 2 weeks, other maternal mental health disorders may be evident.
• Pregnancy and Postpartum Depression (also referred to as maternal depression, peripartum depression, or perinatal depression)- symptoms can start anytime during pregnancy or anytime during the first year postpartum. PSI describes them as: feelings of anger or irritability, lack of interest in baby, appetite and sleep disturbances, crying and sadness, feelings of guilt, shame or hopelessness, loss of interest, joy or pleasure in things you used to enjoy, and/or possible thoughts of harming the baby or yourself. Research shows that around 15% of women experience PPD and it is actually the most common complication of childbirth.
• Pregnancy and Postpartum Anxiety (also referred to as postpartum anxiety, PPA)- the onset of these symptoms occur during or after birth with perinatal anxiety just like perinatal depression. They can consist of constant worry, a feeling/sense of dread that something bad is going to happen (though mother may not be able to identify “what” that bad thing may be), racing thoughts, sleep and appetite disturbances, an inability to sit still, and physical symptoms like dizziness, hot flashes, racing heart.
• Pregnancy and Postpartum Obsessive Compulsive Disorder (also referred to as PPOCD)- this is a form of postpartum anxiety and is the most misunderstood and misdiagnosed perinatal disorders. People think a previous OCD diagnosis is required but this is not the case. As many as 3-5% of new mamas will experience this disorder. Symptoms include obsessions (aka intrusive thoughts), compulsions, a sense of horror about the obsessions, fear of being left alone with the baby, and a hypervigilance in protecting the baby. Moms with this diagnosis also recognize that their thoughts are bizarre and they are very unlikely to act on them. The fact that moms are very troubled by these thoughts and that they want them to stop is an important indicator and distinction between PPOCD (with intrusive thoughts) and Postpartum Psychosis. These thoughts are anxious in nature and not delusional. Obsessions/intrusive thoughts are defined as persistent, repetitive thoughts or mental images related to the baby (or self) that are very upsetting to the mother and not something the mother has ever experienced. Compulsions are repetitive behaviors that the mom feels an urge to do in response to her obsession- i.e. cleaning constantly because mom is worried her baby will get sick and die, or checking the baby constantly during baby’s nap because mom is worried baby will stop breathing, or avoiding walking in the kitchen near knives because mom is worried she may stab the baby.
• Birth Related Post Traumatic Stress Disorder (Postpartum Traumatic Stress Disorder, PPTSD)- PSI defines this disorder as often caused by a frightening or traumatic childbirth or past trauma. It occurs in 9% of women following childbirth. Real or perceived traumas such as prolapsed cord, unplanned C-section, use of vacuum extractor or forceps, baby going to the NICU, feelings of powerlessness, poor communication and/or lack of support and reassurance during the delivery, previous trauma, and severe physical complication or injury during pregnancy or childbirth (postpartum hemorrhage, unexpected hysterectomy, severe preeclampsia/ eclampsia, perineal trauma, or cardiac disease) during delivery or postpartum are most often the cause of PPTSD. Symptoms may include intrusive re-experiencing of a past traumatic event, flashbacks or nightmares, avoidance of stimuli associated with the event (stimuli may include thoughts, feelings, people, places, and details of the event), persistent increased arousal such as irritability, difficulty sleeping, hyper vigilance, exaggerated startle response, anxiety and panic attacks, and feeling a sense of unreality and detachment.
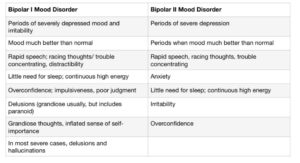
• Bipolar Mood Disorders- many women are diagnosed for the first time ever with bipolar depression or mania in the perinatal period. Informed and thorough assessment and evaluation of past and current mood changes and cycles helps clinicians make the most accurate diagnosis. Criteria for bipolar mood disorder in pregnancy or postpartum can be found here. It’s important that the mother’s mood history is assessed to look for a persistently elevated mood, decreased need for sleep, and periods of over average productivity.
• Postpartum Psychosis- PPP is extremely rare compared to the rates of PPD or PPA- it occurs approximately 1 to 2 out of 1,000 deliveries, .1-.2% of births and the onset is usually sudden and within the first 2 weeks of birth. Symptoms can include delusions or strange beliefs, hallucinations (seeing or hearing things that aren’t there), feeling very irritated, hyperactivity, paranoia and suspiciousness, decreased need for or inability to sleep, rapid mood swings, and difficulty communicating at times. During postpartum psychotic episodes, women experience a break from reality and the delusions and beliefs make sense to her and feel very real. They are often religious. Not all delusions contain violent commands or are of destructive nature. However, it’s IMPERATIVE and VERY IMPORTANT to seek immediate treatment if you suspect PPP in yourself or someone else to ensure no negative action is taken in response to potential dangerous or violent delusions and hallucinations. Many survivors of PPP never experience violent commanding delusions and do not harm themselves of anyone else.
Causes and Risk Factors
Like other mental health disorders, these can be caused by a one OR a combination of biological/physiological, social, and psychological stressors. There are HUGE hormonal changes during and after pregnancy that can lead to chemical changes in the brain resulting in emotional and mental symptoms. Also, lack of social support and connection, family history, and previous experience with these disorders can have significant impact on someone’s risk for diagnosis. However, it’s important to note that previous experience is NOT a requirement. These disorders can occur during or after any pregnancy for a woman, regardless of which pregnancy it may be in her life- first, second, fifth, etc. Biological sex is NOT a requirement for diagnosis either. Fathers can experience symptoms too as mentioned in the beginning of this article.
Treatment
There’s good news folks—parents can feel and get better!! Risk for PMADs can also be reduced and sometimes even prevented with treatment. Treatment options include talk therapy, pharmacological interventions (under an experienced perinatal doctor or psychiatrist’s supervision), and support groups (local or online). Specific therapeutic interventions such as ACT (Acceptance and Commitment Therapy), CBT (Cognitive Behavioral Therapy), person-centered counseling, TF-CBT (trauma focused cognitive behavioral therapy), and EMDR (Eye Movement Desensitization and Reprocessing) have been shown to be effective in helping parents recover from PMADs and ultimately thrive as a parent (Clinical Guideline 197, 2014 from the National Institute for Health and Care Excellence). Our therapists here at Doors of Hope have experience in these treatment modalities and welcome anyone seeking help and support for these unique yet very common issues.
Please see the RESOURCES list below to find local and online resources if you or a loved one is dealing with any perinatal mood or anxiety disorders or symptoms and remember that here at Doors of Hope we have therapists who specialize in postpartum depression and maternal mental health. Give us a call today.
Resources
*Postpartum Support International- an AMAZING organization that offers an
abundance of support via a provider directory list, online support groups, online/ telephone support, a telephone helpline, loss and grief resources, and peer mentor programs.
PSI Helpline- 1.800.944.4773 (phone and texting number) 1.971.203.7773 (text en Español)
*20/20 Mom- a national non-profit social change organization dedicated to closing the gaps in maternal mental health care.
https://www.2020mom.org/our-work
*Psychology Today- an online database to assist in finding a mental health provider (therapist, psychiatrist, etc.). Filters can be applied to assist in finding a provider who specializes in maternal mental health and PMADs. www.psychologytoday.com
CRISIS/EMERGENCY HELP– **if support is needed for those who are suicidal or in severe distress**
The National Suicide Prevention Lifeline- The Lifeline is a US-based suicide prevention network of over 160 crisis centers that provides 24 hour 7 day-a-week live service with a trained counselor, via a toll-free hotline with the number: 1.800.273.8255. A chat feature is available on the website: https:// suicidepreventionlifeline.org/
CALL 911/THE POLICE —————————————————————————————————
REFERENCES
National Institute for Health and Care Excellence (NICE) (2014). Antenatal and postnatal mental health: Clinical management and service guidance. (Clinical Guideline 197) 2014.
http://www.nice.org.uk/guidance/cg192
https://www.2020mom.org/mmh-disorders – https://www.postpartum.net/learn-more/ https://americanpregnancy.org/healthy-pregnancy/first-year-of-life/baby-blues/

